History of medicine
All human societies have medical beliefs that provide explanations for birth, death, and disease. Throughout history, illness has been attributed to witchcraft, demons, adverse astral influence, or the will of the gods. These ideas still retain some power, with faith healing and shrines still used in some places, although the rise of scientific medicine over the past millennium has altered or replaced mysticism in most cases.
| History of science |
 |
| Background |
|---|
| Theories/sociology |
| Historiography |
| Pseudoscience |
| By era |
| In early cultures |
| in Classical Antiquity |
| In the Middle Ages |
| In the Renaissance |
| Scientific Revolution |
| Romanticism in science |
| By culture |
| Arabic-Islamic |
| Medieval Byzantine |
| Chinese |
| Indian |
| African |
| By topic |
| Natural sciences |
| Astronomy |
| Biology |
| Botany |
| Chemistry |
| Ecology |
| Geology |
| Paleontology |
| Physics |
| Mathematics |
| Algebra |
| Calculus |
| Combinatorics |
| Geometry |
| Logic |
| Probability |
| Statistics |
| Trigonometry |
| Social sciences |
| Anthropology |
| Economics |
| Geography |
| Linguistics |
| Political science |
| Psychology |
| Sociology |
| Sustainability |
| Technology |
| Agricultural science |
| Computer science |
| Materials science |
| Medicine |
| Navigational pages |
| Timelines |
| Portal |
| Categories |
Contents |
Prehistoric medicine
Although there is no record to establish when plants were first used for medicinal purposes (herbalism), the use of plants as healing agents is an ancient practice. Over time through emulation of the behavior of fauna a medicinal knowledge base developed and was passed between generations. As tribal culture specialized specific castes, Shamans and apothecaries performed the 'niche occupation' of healing.
Antiquity
Egypt
Ancient Egypt developed a large, varied and fruitful medical tradition. Herodotus described the Egyptians as "the healthiest of all men, next to the Libyans",[1] due to the dry climate and the notable public health system that they possessed. According to him, "[t]he practice of medicine is so specialized among them that each physician is a healer of one disease and no more." Although Egyptian medicine, to a good extent, dealt with the supernatural,[2] it eventually developed a practical use in the fields of anatomy, public health, and clinical diagnostics.
Medical information in the Edwin Smith Papyrus[3] may date to a time as early as 3000 BC.[4] The earliest known surgery in Egypt was performed in Egypt around 2750 BC. Imhotep in the 3rd dynasty is sometimes credited with being the founder of ancient Egyptian medicine and with being the original author of the Edwin Smith Papyrus, detailing cures, ailments and anatomical observations. The Edwin Smith Papyrus is regarded as a copy of several earlier works and was written circa 1600 BC. It is an ancient textbook on surgery almost completely devoid of magical thinking and describes in exquisite detail the examination, diagnosis, treatment, and prognosis of numerous ailments.[5]
Conversely, the Ebers papyrus[6] (c. 1550 BC) is full of incantations and foul applications meant to turn away disease-causing demons, and other superstition. The Ebers papyrus also provides our earliest possible documentation of ancient awareness of tumors, but ancient medical terminology being badly understood, cases Ebers 546 and 547 for instance may refer to simple swellings.
The Kahun Gynaecological Papyrus[7] treats women's complaints, including problems with conception. Thirty four cases detailing diagnosis and treatment survive, some of them fragmentarily.[8] Dating to 1800 BC, it is the oldest surviving medical text of any kind.
Medical institutions, referred to as Houses of Life are known to have been established in ancient Egypt as early as the 1st Dynasty.[9] By the time of the 19th Dynasty some workers enjoyed such benefits as medical insurance, pensions and sick leave.[9]
The earliest known physician is also credited to ancient Egypt: Hesy-Ra, “Chief of Dentists and Physicians” for King Djoser in the 27th century BC.[9] Also, the earliest known woman physician, Peseshet, practiced in Ancient Egypt at the time of the 4th dynasty. Her title was “Lady Overseer of the Lady Physicians.” In addition to her supervisory role, Peseshet trained midwives at an ancient Egyptian medical school in Sais.[9]
Mesopotamia and Levant
- Further information: Babylonia - Medicine
The oldest Babylonian texts on medicine date back to the Old Babylonian period in the first half of the 2nd millennium BC. The most extensive Babylonian medical text, however, is the Diagnostic Handbook written by the physician Esagil-kin-apli of Borsippa,[10] during the reign of the Babylonian king Adad-apla-iddina (1069-1046 BC).[11]
Along with contemporary ancient Egyptian medicine, the Babylonians introduced the concepts of diagnosis, prognosis, physical examination, and medical prescriptions. In addition, the Diagnostic Handbook introduced the methods of therapy and etiology and the use of empiricism, logic and rationality in diagnosis, prognosis and therapy. The text contains a list of medical symptoms and often detailed empirical observations along with logical rules used in combining observed symptoms on the body of a patient with its diagnosis and prognosis.[12]
The Diagnostic Handbook was based on a logical set of axioms and assumptions, including the modern view that through the examination and inspection of the symptoms of a patient, it is possible to determine the patient's disease, its aetiology and future development, and the chances of the patient's recovery. The symptoms and diseases of a patient were treated through therapeutic means such as bandages, creams and pills.[10]
Most of our knowledge of ancient Hebrew medicine during the 1st millennium BCE comes from the Torah, i.e. the Five Books of Moses, which contain various health related laws and rituals, such as isolating infected people (Leviticus 13:45-46), washing after handling a dead body (Numbers 19:11-19) and burying excrement away from camp (Deuteronomy 23:12-13). While the observance of these statutes would have and do lead to several health benefits, Jewish belief commands that these rituals and prohibitions be kept purely to fulfill the will of God with no ulterior motive. Max Neuberger, writing in his "History of Medicine" says
- "The commands concern prophylaxis and suppression of epidemics, suppression of venereal disease and prostitution, care of the skin, baths , food, housing and clothing, regulation of labor , sexual life , discipline of the people , etc. Many of these commands, such as Sabbath rest, circumcision, laws concerning food (interdiction of blood and pork), measures concerning menstruating and lying-in women and those suffering from gonorrhea, isolation of lepers, and hygiene of the camp, are, in view of the conditions of the climate, surprisingly rational."(Neuburger: History of Medicine, Oxford University Press, 1910, Vol. I, p. 38).
India
The Atharvaveda, a sacred text of Hinduism dating from the Early Iron Age, is the first Indian text dealing with medicine, like the medicine of the Ancient Near East based on concepts of the exorcism of demons and magic. The Atharvaveda also contain prescriptions of herbs for various ailments. The use of herbs to treat ailments would later form a large part of Ayurveda.
In the first millennium BCE, the worlds first scientific system of medicine emerges known as Ayurveda, literally meaning the science of life. Ayurveda is the literate, scholarly system of medicine that originated in post-Vedic India. Its two most famous texts belong to the schools of Charaka, born c. 600 BCE, and Sushruta, born 600 BCE. While these writings display some limited continuities with the earlier medical ideas known from the Vedas, historians have been able to demonstrate direct historical connections between early Ayurveda and the early literature of the Buddhists and Jains. The earliest foundations of Ayurveda were built on a synthesis of traditional herbal practices together with a massive addition of theoretical conceptualizations, new nosologies and new therapies dating from about 400 BCE onwards, and coming out of the communities of thinkers who included the Buddha and others.[13].
According to the compendium of Charaka, the Charakasamhitā, health and disease are not predetermined and life may be prolonged by human effort. The compendium of Suśruta, the Suśrutasamhitā defines the purpose of medicine to cure the diseases of the sick, protect the healthy, and to prolong life. Both these ancient compendia include details of the examination, diagnosis, treatment, and prognosis of numerous ailments. The Suśrutasamhitā is notable for describing procedures on various forms of surgery, including rhinoplasty, the repair of torn ear lobes, perineal lithotomy, cataract surgery, and several other excisions and other surgical procedures. Most remarkable is Sushruta's penchant for scientific classification: His medical treatise consists of 184 chapters, 1,120 conditions are listed, including injuries and illnesses relating to ageing and mental illness. The Sushruta Samhita describe 125 surgical instrument, 300 surgical procedures and classifies human surgery in 8 categories [4]
The Ayurvedic classics mention eight branches of medicine: kāyācikitsā (internal medicine), śalyacikitsā (surgery including anatomy), śālākyacikitsā (eye, ear, nose, and throat diseases), kaumārabhṛtya (pediatrics), bhūtavidyā (spirit medicine), and agada tantra (toxicology), rasāyana (science of rejuvenation), and vājīkaraṇa (aphrodesiacs, mainly for men). Apart from learning these, the student of Āyurveda was expected to know ten arts that were indispensable in the preparation and application of his medicines: distillation, operative skills, cooking, horticulture, metallurgy, sugar manufacture, pharmacy, analysis and separation of minerals, compounding of metals, and preparation of alkalis. The teaching of various subjects was done during the instruction of relevant clinical subjects. For example, teaching of anatomy was a part of the teaching of surgery, embryology was a part of training in pediatrics and obstetrics, and the knowledge of physiology and pathology was interwoven in the teaching of all the clinical disciplines. The normal length of the student's training appears to have been seven years. But the physician was to continue to learn.[14]
China
China also developed a large body of traditional medicine. Much of the philosophy of traditional Chinese medicine derived from empirical observations of disease and illness by Taoist physicians and reflects the classical Chinese belief that individual human experiences express causative principles effective in the environment at all scales. These causative principles, whether material, essential, or mystical, correlate as the expression of the natural order of the universe.
The foundational text of Chinese medicine is the Huangdi neijing, or Yellow Emperor's Inner Canon, which is composed of two books: the Suwen 素問 ("Basic Questions") and the Lingshu 靈樞 ("Divine Pivot"). Although the Neijing has long been attributed to the mythical Yellow Emperor (twenty-seventh century BC), Chinese scholars started doubting this attribution as early as the eleventh century and now usually date the Neijing to the late Warring States period (5th century-221 BC).[15] Because the medical "silk manuscripts" dating from around 200 BC that were excavated in the 1970s from the tomb of a Han-dynasty noble in Mawangdui are undoubtedly ancestors of the received Neijing, scholars like Nathan Sivin now argue that the Neijing was first compiled in the 1st century BC.[16]
In 56 BC, Zhang Liang invented an instrument named "Meng" which is considered to be precursor of modern stethoscope.[17]
During the Han dynasty, Zhang Zhongjing, who was mayor of Changsha near the end of the second century A.D., wrote a Treatise on Cold Damage, which contains the earliest known reference to the Neijing Suwen. The Jin Dynasty practitioner and advocate of acupuncture and moxibustion, Huangfu Mi (215-282 A.D), also quotes the Yellow Emperor in his Jiayi jing, ca. 265 A.D. During the Tang Dynasty, Wang Bing claimed to have located a copy of the originals of the Suwen, which he expanded and edited substantially. This work was revisited by an imperial commission during the eleventh century A.D., and the result is our best extant representation of the foundational roots of traditional Chinese medicine.
Greek and Roman medicine

The first known Greek medical school opened in Cnidus in 700 BC. Alcmaeon, author of the first anatomical work, worked at this school, and it was here that the practice of observing patients was established. As was the case elsewhere, the ancient Greeks developed a humoral medicine system where treatment sought to restore the balance of humours within the body.
Temples dedicated to the healer-god Asclepius, known as Asclepieia (Greek: Ἀσκληπιεῖα, sing. Ἀσκληπιεῖον, 'Asclepieion), functioned as centers of medical advice, prognosis, and healing.[18] At these shrines, patients would enter a dream-like state of induced sleep known as "enkoimesis" (Greek: ενκοίμησις) not unlike anesthesia, in which they either received guidance from the deity in a dream or were cured by surgery.[19] Asclepeia provided carefully controlled spaces conducive to healing and fulfilled several of the requirements of institutions created for healing.[18] In the Asclepieion of Epidaurus, three large marble boards dated to 350 BC preserve the names, case histories, complaints, and cures of about 70 patients who came to the temple with a problem and shed it there. Some of the surgical cures listed, such as the opening of an abdominal abscess or the removal of traumatic foreign material, are realistic enough to have taken place, but with the patient in a state of enkoimesis induced with the help of soporific substances such as opium.[19]
A towering figure in the history of medicine was the physician Hippocrates of Kos (ca. 460 BC – ca. 370 BC), considered the "father of modern medicine."[20][21] The Hippocratic Corpus is a collection of around seventy early medical works from ancient Greece strongly associated with Hippocrates and his students. Most famously, Hippocrates invented the Hippocratic Oath for physicians, which is still relevant and in use today.
Hippocrates and his followers were first to describe many diseases and medical conditions. He is given credit for the first description of clubbing of the fingers, an important diagnostic sign in chronic suppurative lung disease, lung cancer and cyanotic heart disease. For this reason, clubbed fingers are sometimes referred to as "Hippocratic fingers".[22] Hippocrates was also the first physician to describe Hippocratic face in Prognosis. Shakespeare famously alludes to this description when writing of Falstaff's death in Act II, Scene iii. of Henry V.[23][24]
Hippocrates began to categorize illnesses as acute, chronic, endemic and epidemic, and use terms such as, "exacerbation, relapse, resolution, crisis, paroxysm, peak, and convalescence."[25][26] Another of Hippocrates's major contributions may be found in his descriptions of the symptomatology, physical findings, surgical treatment and prognosis of thoracic empyema, i.e. suppuration of the lining of the chest cavity. His teachings remain relevant to present-day students of pulmonary medicine and surgery.[27] Hippocrates was the first documented chest surgeon and his findings are still valid.[27]

Herophilus of Chalcedon, working at the medical school of Alexandria placed intelligence in the brain, and connected the nervous system to motion and sensation. Herophilus also distinguished between veins and arteries, noting that the latter pulse while the former do not. He and his contemporary, Erasistratus of Chios, researched the role of veins and nerves, mapping their courses across the body. Erasistratus connected the increased complexity of the surface of the human brain compared to other animals to its superior intelligence. He sometimes employed experiments to further his research, at one time repeatedly weighing a caged bird, and noting its weight loss between feeding times. In Erasistratus' physiology, air enters the body, is then drawn by the lungs into the heart, where it is transformed into vital spirit, and is then pumped by the arteries throughout the body. Some of this vital spirit reaches the brain, where it is transformed into animal spirit, which is then distributed by the nerves.[29]
The Greek Galen was one of the greatest surgeons of the ancient world and performed many audacious operations—including brain and eye surgeries— that were not tried again for almost two millennia. Later, in medieval Europe, Galen's writings on anatomy became the mainstay of the medieval physician's university curriculum along; but they suffered greatly from stasis and intellectual stagnation. In the 1530s, however, Belgian anatomist and physician Andreas Vesalius took on a project to translate many of Galen's Greek texts into Latin. Vesalius's most famous work, De humani corporis fabrica, was greatly influenced by Galenic writing and form.[30] The works of Galen and Avicenna, especially The Canon of Medicine which incorporated the teachings of both, were translated into Latin, and the Canon remained the most authoritative text on anatomy in European medical education until the 16th century.
The Romans invented numerous surgical instruments, including the first instruments unique to women,[31] as well as the surgical uses of forceps, scalpels, cautery, cross-bladed scissors, the surgical needle, the sound, and speculas.[32][33] Romans were also pioneers in cataract surgery.[34]
Medieval medicine was an evolving mixture of the scientific and the spiritual like Unani. In the early Middle Ages, following the fall of the Roman Empire, standard medical knowledge was based chiefly upon surviving Greek and Roman texts, preserved in monasteries and elsewhere. Ideas about the origin and cure of disease were not, however, purely secular, but were also based on a spiritual world view, in which factors such as destiny, sin, and astral influences played as great a part as any physical cause.
Oribasius was the greatest Byzantine compiler of medical knowledge. Several of his works, along with many other Byzantine physicians, were translated into Latin, and eventually, during the Enlightenment and Age of Reason, into English and French. The last great Byzantine Physician was John Actuarius, who lived in the early 14th century in Constantinople.
Middle Ages
Islamic Middle Ages
Persia's position at the crossroads of the East and the West frequently placed it in the midst of developments in both ancient Greek and Indian medicine. The first generation of Persian physicians was trained at the Academy of Jundishapur. This evolved into the medieval Islamic Bimaristan hospitals.[35][36]
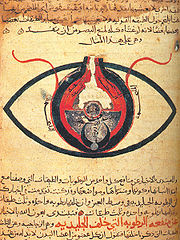
The Islamic civilization rose to primacy in medical science as Muslim physicians contributed significantly to the field of medicine, including anatomy, ophthalmology, pharmacology, pharmacy, physiology, surgery, and the pharmaceutical sciences. The Arabs were influenced by, and further developed Greek, Roman and Indian medical practices. Galen, Hippocrates, Sushruta and Charaka were pre-eminent authorities.[37] The translation of 129 works of ancient Greek physician Galen into Arabic by Hunayn ibn Ishaq and his assistants, and in particular Galen's insistence on a rational systematic approach to medicine, set the template for Islamic medicine, which rapidly spread throughout the Arab Empire. Muslim physicians set up some of the earliest dedicated hospitals, which later spread to Europe during the Crusades, inspired by the hospitals in the Middle East.[38]
Muhammad ibn Zakariya al-Razi became the first physician to systematically use alcohol in his practice as a physician. The Comprehensive Book of Medicine (Large Comprehensive, Hawi, "al-Hawi" or "The Continence") was written by the Iranian chemist Muhammad ibn Zakariya al-Razi, the "Large Comprehensive" was the most sought after of all his compositions. In it, Muhammad ibn Zakariya al-Razi recorded clinical cases of his own experience and provided very useful recordings of various diseases. The "Kitab fi al-jadari wa-al-hasbah" by Muhammad ibn Zakariya al-Razi, with its introduction on measles and smallpox was also very influential in Europe.
Al-Kindi wrote De Gradibus, in which he demonstrated the application of mathematics to medicine, particularly in the field of pharmacology. This includes the development of a mathematical scale to quantify the strength of drugs, and a system that would allow a doctor to determine in advance the most critical days of a patient's illness.[39] Razi (Rhazes) (865-925) recorded clinical cases of his own experience and provided very useful recordings of various diseases. His Comprehensive Book of Medicine, which introduced measles and smallpox, was very influential in Europe.
Abu al-Qasim (Abulcasis), regarded as the father of modern surgery,[40] wrote the Kitab al-Tasrif (1000), a 30-volume medical encyclopedia which was taught at Muslim and European medical schools until the 17th century. He used numerous surgical instruments, including some that are unique to women.[31][41]
Avicenna, considered among the most influential medical scholars in history,[38] wrote The Canon of Medicine (1025) and The Book of Healing (1027), which remained standard textbooks in both Muslim and European universities until the 17th century. Avicenna's contributions include the discovery of the contagious nature of infectious diseases, the introduction of quarantine to limit the spread of contagious diseases, the introduction of experimental medicine and clinical trials,[42] the first descriptions on bacteria and viral organisms,[43] the distinction of mediastinitis from pleurisy, the contagious nature of phthisis and tuberculosis, the distribution of diseases by water and soil, and the first careful descriptions of skin troubles, sexually transmitted diseases, and nervous ailments,[38] as well the use of ice to treat fevers, and the separation of medicine from pharmacology, which was important to the development of the pharmaceutical sciences.[41]
In 1242, Ibn al-Nafis was the first to describe pulmonary circulation and coronary circulation,[44] which form the basis of the circulatory system, for which he is considered the father of the theory of circulation.[45] He also described the earliest concept of metabolism,[46] and developed new systems of physiology to replace the Avicennian and Galenic systems, while discrediting many of their erroneous theories on the four humours, pulsation,[47] bones, muscles, intestines, sensory organs, bilious canals, esophagus, stomach, etc.[48]
The Tashrih al-badan (Anatomy of the body) of Mansur ibn Ilyas (c. 1390) contained comprehensive diagrams of the body's structural, nervous and circulatory systems.[49] During the Black Death, or bubonic plague in 14th century al-Andalus, Ibn Khatima and Ibn al-Khatib discovered that infecious diseases are caused by microorganisms which enter the human body.[50] Other medical innovations first introduced by Muslim physicians include the discovery of the immune system, the introduction of microbiology, the use of animal testing, and the combination of medicine with other sciences (including agriculture, botany, chemistry, and pharmacology),[41] as well as the invention of the injection syringe by Ammar ibn Ali al-Mawsili in 9th century Iraq, the first drugstores in Baghdad (754), the distinction between medicine and pharmacy by the 12th century, and the discovery of at least 2,000 medicinal and chemical substances.[51]
Christian Middle Ages


In western Europe, with the collapse of Roman imperial authority, medicine became localised; folk-medicine supplemented what remained of the medical knowledge of antiquity. Medical knowledge was preserved and practised in many monastic institutions, which often had a hospital attached. Organised professional medicine re-emerged, with the foundation of the medical college (Schola Medica Salernitana) of Salerno in Italy in the 11th century, which in co-operation with the monastery of Monte Cassino, translated many Byzantine and Arabic works. In the twelfth century universities were founded in Italy and elsewhere, which soon developed schools of medicine.
Gradually the reliance on the masters of the ancient world was augmented by the results of individual observation and experience. Surgical practice improved greatly during the medieval period. Rogerius Salernitanus composed his Chirurgia, which became the foundation for modern Western surgical manuals up to the modern time.
Renaissance to Early Modern period
With the Renaissance came an increase in experimental investigation, principally in dissection and examining bodies. The work of individuals like Andreas Vesalius and William Harvey challenged accepted folklore with scientific evidence. The development of modern neurology began in the 16th century with Vesalius, who described the anatomy of the brain and much else; he had little notion of function, thinking that it lay mainly in the ventricles. Understanding and diagnosis improved but with little direct benefit to health. Few effective drugs existed, beyond opium and quinine. Folklore cures and potentially poisonous metal-based compounds were popular treatments.
Modern medicine
Medicine was revolutionized in the 19th century and beyond by advances in chemistry and laboratory techniques and equipment, old ideas of infectious disease epidemiology were replaced with bacteriology and virology.
Bacteria and microorganisms were first observed with a microscope by Antonie van Leeuwenhoek in 1676, initiating the scientific field microbiology.[52]
Ignaz Semmelweis (1818–1865) in 1847 dramatically reduced the death rate of new mothers from childbed fever by the simple expedient of requiring physicians to clean their hands before attending to women in childbirth. His discovery pre-dated the germ theory of disease. However, his discoveries were not appreciated by his contemporaries and came into general use only with discoveries of British surgeon Joseph Lister, who in 1865 proved the principles of antisepsis in the treatment of wounds; However, medical conservatism on new breakthroughs in pre-existing science prevented them from being generally well received during the 19th century.
After Charles Darwin's 1859 publication of The Origin of Species, Gregor Mendel (1822–1884) published in 1865 his books on pea plants, which would be later known as Mendel's laws. Re-discovered at the turn of the century, they would form the basis of classical genetics. The 1953 discovery of the structure of DNA by Watson and Crick would open the door to molecular biology and modern genetics. During the late 19th century and the first part of the 20th century, several physicians, such as Nobel prize winner Alexis Carrel, supported eugenics, a theory first formulated in 1865 by Francis Galton. Eugenics was discredited as a science after the Nazis' experiments in World War II became known; however, compulsory sterilization programs continued to be used in modern countries (including the US, Sweden and Peru) until much later.
Semmelweis's work was supported by the discoveries made by Louis Pasteur. Linking microorganisms with disease, Pasteur brought about a revolution in medicine. He also invented with Claude Bernard (1813–1878) the process of pasteurization still in use today. His experiments confirmed the germ theory. Claude Bernard aimed at establishing scientific method in medicine; he published An Introduction to the Study of Experimental Medicine in 1865. Beside this, Pasteur, along with Robert Koch (who was awarded the Nobel Prize in 1905), founded bacteriology. Koch was also famous for the discovery of the tubercle bacillus (1882) and the cholera bacillus (1883) and for his development of Koch's postulates.
The participation of women in medical care (beyond serving as midwives, sitters and cleaning women) was brought about by the likes of Florence Nightingale. These women showed a previously male dominated profession the elemental role of nursing in order to lessen the aggravation of patient mortality which resulted from lack of hygiene and nutrition. Nightingale set up the St Thomas hospital, post-Crimea, in 1852. Elizabeth Blackwell (1821–1910) became the first woman to formally study, and subsequently practice, medicine in the United States.
It was in this era that actual cures were developed for certain endemic infectious diseases. However the decline in many of the most lethal diseases was more due to improvements in public health and nutrition than to medicine. It was not until the 20th century that the application of the scientific method to medical research began to produce multiple important developments in medicine, with great advances in pharmacology and surgery.
During the 1910s, medicine was closely related to church in most of Europe including the United Kingdom. Most doctors took permission of the church before prescribing any medicine to patients.[17] Before surgeries, permission of the church was mandatory.[17] During the First World War, Alexis Carrel and Henry Dakin developed the Carrel-Dakin method of treating wounds with an irrigation, Dakin's solution, a germicide which helped prevent gangrene.
The Great War spurred the usage of Roentgen's X-ray, and the electrocardiograph, for the monitoring of internal bodily functions. This was followed in the inter-war period by the development of the first anti-bacterial agents such as the sulpha antibiotics. The Second World War saw the introduction of widespread and effective antimicrobial therapy with the development and mass production of penicillin antibiotics, made possible by the pressures of the war and the collaboration of British scientists with the American pharmaceutical industry.
Lunatic asylums began to appear in the Industrial Era. Emil Kraepelin (1856–1926) introduced new medical categories of mental illness, which eventually came into psychiatric usage despite their basis in behavior rather than pathology or etiology. In the 1920s surrealist opposition to psychiatry was expressed in a number of surrealist publications. In the 1930s several controversial medical practices were introduced including inducing seizures (by electroshock, insulin or other drugs) or cutting parts of the brain apart (leucotomy or lobotomy). Both came into widespread use by psychiatry, but there were grave concerns and much opposition on grounds of basic morality, harmful effects, or misuse. In the 1950s new psychiatric drugs, notably the antipsychotic chlorpromazine, were designed in laboratories and slowly came into preferred use. Although often accepted as an advance in some ways, there was some opposition, due to serious adverse effects such as tardive dyskinesia. Patients often opposed psychiatry and refused or stopped taking the drugs when not subject to psychiatric control. There was also increasing opposition to the use of psychiatric hospitals, and attempts to move people back into the community on a collaborative user-led group approach ("therapeutic communities") not controlled by psychiatry. Campaigns against masturbation were done in the Victorian era and elsewhere. Lobotomy was used until the 1970s to treat schizophrenia. This was denounced by the anti-psychiatric movement in the 1960s and later.
The 20th century witnessed a shift from a master-apprentice paradigm of teaching of clinical medicine to a more "democratic" system of medical schools. With the advent of the evidence-based medicine and great advances of information technology the process of change is likely to evolve further, with greater development of international projects such as the Human genome project.
In 1954 Joseph Murray, J. Hartwell Harrison, M.D. and others accomplished the first kidney transplantation.
Notes
- ↑ Herodotus. "Chapter 77, Book II" (in English translation). The Histories.
- ↑ Nunn, John F. (2002). Ancient Egyptian Medicine. University of Oklahoma Press.
- ↑ J. H. Breasted, The Edwin Smith Surgical Papyrus, University of Chicago Press, 1930
- ↑ Medicine in Ancient Egypt 1
- ↑ Edwin Smith papyrus - Britannica Online Encyclopedia
- ↑ P. W. Bryan, The Papyrus Ebers, Geoffrey Bles: London, 1930
- ↑ Griffith, F. Ll. The Petrie Papyri: Hieratic Papyri from Kahun and Gurob
- ↑ The Kahun Gynaecological Papyrus
- ↑ 9.0 9.1 9.2 9.3 Medicine in Ancient Egypt by Sameh M. Arab, MD
- ↑ 10.0 10.1 H. F. J. Horstmanshoff, Marten Stol, Cornelis Tilburg (2004), Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine, p. 99, Brill Publishers, ISBN 90-04-13666-5.
- ↑ Marten Stol (1993), Epilepsy in Babylonia, p. 55, Brill Publishers, ISBN 90-72371-63-1.
- ↑ H. F. J. Horstmanshoff, Marten Stol, Cornelis Tilburg (2004), Magic and Rationality in Ancient Near Eastern and Graeco-Roman Medicine, p. 97-98, Brill Publishers, ISBN 90-04-13666-5.
- ↑ Kenneth G. Zysk, Asceticism and Healing in Ancient India: Medicine in the Buddhist Monastery, Oxford University Press, rev. ed. (1998) ISBN 0-19-505956-5
- ↑ Dominik Wujastyk, ed., The Roots of Ayurveda, Penguin (2003) ISBN 0-14-044824-1
- ↑ Unschuld (2003), 1.
- ↑ Sivin (1993).
- ↑ 17.0 17.1 17.2 Arturo Castiglioni (1958). A history of medicine. Kessinger Publishing. pp. 36.
- ↑ 18.0 18.1 Risse, G.B. Mending bodies, saving souls: a history of hospitals. Oxford University Press, 1990. p. 56 [1]
- ↑ 19.0 19.1 Askitopoulou, H., Konsolaki, E., Ramoutsaki, I., Anastassaki, E. Surgical cures by sleep induction as the Asclepieion of Epidaurus. The history of anesthesia: proceedings of the Fifth International Symposium, by José Carlos Diz, Avelino Franco, Douglas R. Bacon, J. Rupreht, Julián Alvarez. Elsevier Science B.V., International Congress Series 1242(2002), p.11-17. [2]
- ↑ Hippocrates: The "Greek Miracle" in Medicine
- ↑ The Father of Modern Medicine: Hippocrates
- ↑ Schwartz, Richards & Goyal 2006
- ↑ Singer & Underwood 1962, p. 40
- ↑ Margotta 1968, p. 70
- ↑ Garrison 1966, p. 97
- ↑ Martí-Ibáñez 1961, p. 90
- ↑ 27.0 27.1 Major 1965
- ↑ Day, Cyrus L. (1967). Quipus and Witches' Knots. Lawrence, Kansas: University of Kansas Press. pp. 86–89, 124–126.
- ↑ Mason, A History of the Sciences, p 57
- ↑ Dear, Peter. Revolutionizing the Sciences: European Knowledge and Its Ambitions, 1500-1700. Princeton, NJ: Princeton University Press (2001), 37-39.
- ↑ 31.0 31.1 Surgical Instruments from Ancient Rome
- ↑ Roman period surgery set on show, BBC
- ↑ William Alexander Greenhill, Chirurgia
- ↑ The Romans carried out cataract ops, BBC
- ↑ Micheau, Françoise, "The Scientific Institutions in the Medieval Near East", pp. 991–2, in (Morelon & Rashed 1996, pp. 985-1007)
- ↑ Peter Barrett (2004), Science and Theology Since Copernicus: The Search for Understanding, p. 18, Continuum International Publishing Group, ISBN 056708969X.
- ↑ Amber Haque (2004), "Psychology from Islamic Perspective: Contributions of Early Muslim Scholars and Challenges to Contemporary Muslim Psychologists", Journal of Religion and Health 43 (4): 357-377 [361]
- ↑ 38.0 38.1 38.2 George Sarton, Introduction to the History of Science.
(cf. Dr. A. Zahoor and Dr. Z. Haq (1997), Quotations From Famous Historians of Science, Cyberistan. - ↑ Felix Klein-Frank (2001), Al-Kindi, in Oliver Leaman and Hossein Nasr, History of Islamic Philosophy, p. 172. Routledge, London.
- ↑ A. Martin-Araguz, C. Bustamante-Martinez, Ajo V. Fernandez-Armayor, J. M. Moreno-Martinez (2002). "Neuroscience in al-Andalus and its influence on medieval scholastic medicine", Revista de neurología 34 (9), p. 877-892.
- ↑ 41.0 41.1 41.2 Bashar Saad, Hassan Azaizeh, Omar Said (October 2005). "Tradition and Perspectives of Arab Herbal Medicine: A Review", Evidence-based Complementary and Alternative Medicine 2 (4), p. 475-479 [476]. Oxford University Press.
- ↑ David W. Tschanz, MSPH, PhD (August 2003). "Arab Roots of European Medicine", Heart Views 4 (2).
- ↑ The Canon of Medicine, The American Institute of Unani Medicine, 2003.
- ↑ Husain F. Nagamia (2003), "Ibn al-Nafīs: A Biographical Sketch of the Discoverer of Pulmonary and Coronary Circulation", Journal of the International Society for the History of Islamic Medicine 1, p. 22–28.
- ↑ Chairman's Reflections (2004), "Traditional Medicine Among Gulf Arabs, Part II: Blood-letting", Heart Views 5 (2), p. 74-85 [80].
- ↑ Dr. Abu Shadi Al-Roubi (1982), "Ibn Al-Nafis as a philosopher", Symposium on Ibn al-Nafis, Second International Conference on Islamic Medicine: Islamic Medical Organization, Kuwait (cf. Ibn al-Nafis As a Philosopher, Encyclopedia of Islamic World).
- ↑ Nahyan A. G. Fancy (2006), "Pulmonary Transit and Bodily Resurrection: The Interaction of Medicine, Philosophy and Religion in the Works of Ibn al-Nafīs (died 1288)", p. 3 & 6, Electronic Theses and Dissertations, University of Notre Dame.[3]
- ↑ Dr. Sulaiman Oataya (1982), "Ibn ul Nafis has dissected the human body", Symposium on Ibn al-Nafis, Second International Conference on Islamic Medicine: Islamic Medical Organization, Kuwait (cf. Ibn ul-Nafis has Dissected the Human Body, Encyclopedia of Islamic World).
- ↑ H. R. Turner (1997), p. 136—138.
- ↑ Ibrahim B. Syed, Ph.D. (2002). "Islamic Medicine: 1000 years ahead of its times", Journal of the Islamic Medical Association 2, p. 2-9.
- ↑ Information taken from the abstract of Hadzović, S (1997). "[Pharmacy and the great contribution of Arab-Islamic science to its development] (Article in Croatian)". Medicinski arhiv 51 (1–2): 47–50. ISSN 0350-199X. PMID 9324574.
- ↑ Madigan M, Martinko J (editors) (2006). Brock Biology of Microorganisms (11th ed.). Prentice Hall. ISBN 0-13-144329-1.
References
- Murray, Joseph E., "The First Successful Organ Transplants in Man", Nobel Lect., 1990, Nobelprize.org., Web, July 7, 2010
Bibliography
- Porter, R. (1997). The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present. Harper Collins. ISBN 0-00-215173-1.
- Rousseau, George S. (2003). Framing and Imagining Disease in Cultural History (Basingstoke: Palgrave Macmillan). [with Miranda Gill, David Haycock and Malte Herwig]. ISBN 1 – 4039 -1292 - 0
- Sivin, Nathan (1993). "Huang-ti nei-ching 黃帝內經." In Early Chinese Texts: A Bibliographical Guide, ed. by Michael Loewe: 196-215. Institute for East Asian Studies, University of California, Berkeley.
- Unschuld, Paul U. (2003). Huang Di Nei Jing Su Wen: Nature, Knowledge, Imagery in an Ancient Chinese Medical Text. Berkeley and Los Angeles: University of California Press.
- Walsh, James J. (1908, reprinted 2003). The Popes and Science; the History of the Papal Relations to Science During the Middle Ages and Down to Our Own Time. Kessinger Publishing. ISBN 0-7661-3646-9. from WorldCat[5] Review excerpts:
See also
- Centers for Disease Control and Prevention timeline
- Timeline of medicine
External links
- American Association for the History of Medicine,
- Science Museum's History of Medicine Website
 "History of Medicine". Catholic Encyclopedia. New York: Robert Appleton Company. 1913.
"History of Medicine". Catholic Encyclopedia. New York: Robert Appleton Company. 1913. "Anatomy". Catholic Encyclopedia. New York: Robert Appleton Company. 1913.
"Anatomy". Catholic Encyclopedia. New York: Robert Appleton Company. 1913.- History of Medicine, United States National Library of Medicine
- Directory of History of Medicine Collections
- The history of medicine and surgery as portrayed by various artists
- Medicine @ JewishEncyclopedia.com
- Exhibition of the Vatican Library's Medical Holdings @ The Library of Congress
- Info Britain - History of medicine in the UK
- Wellcome Library History of Medicine
- Digital Clendening Library at the University of Kansas Medical Center
- "MacKinney Collection of Medieval Medical Illustrations"
- The Center for the History of Medicine, Countway Library, Harvard Medical School (includes the Warren Anatomical Museum)
|
|||||||||||||

